Ian Khan, releases new book Undisrupted during World Economic Forum 2025 in Davos.
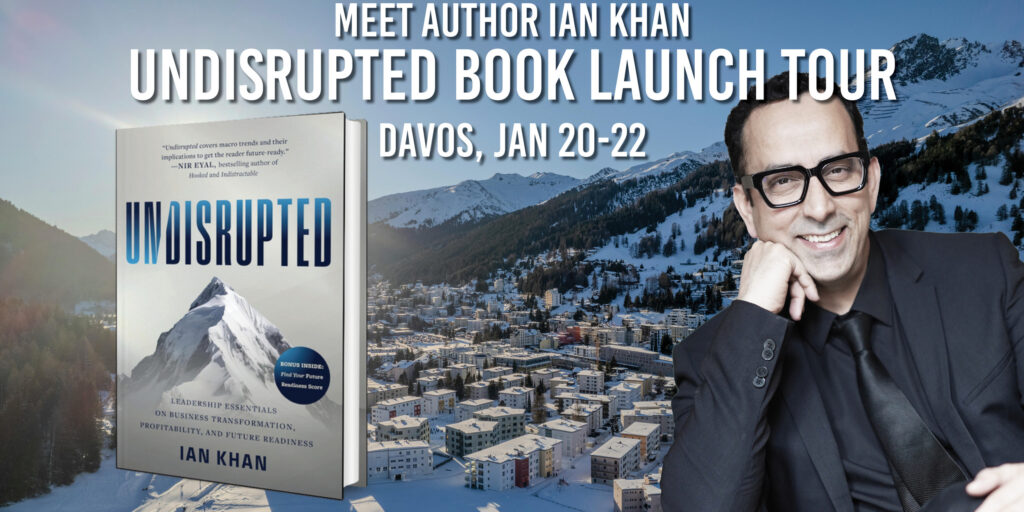
New York, January 17, 2025 – Ian Khan, globally renowned futurist, author, and innovation thought leader, will officially launch his highly anticipated new book, Undisrupted: Leadership Essentials on Business Transformation, Profitability and Future Readiness . As the world grapples with unprecedented technological and societal changes, Khan’s latest work is a timely and essential guide for individuals, organizations, and governments seeking to navigate disruption and thrive in a fast-evolving landscape.
A Book for Today and Tomorrow
Undisrupted is more than a book—it’s a movement to empower everyone to shape the future rather than fear it. Introducing the revolutionary Future Readiness Score, the book equips readers to measure their adaptability to disruption, offering a seven point stragy to transform fear and vulnerability to purpose, profits and embracing emerging trends and unlock opportunities.
From the rise of EVs and the creator economy to global initiatives like Saudi Arabia’s NEOM and the UAE’s trailblazing sustainability efforts, Undisrupted demystifies the forces shaping tomorrow. It brings stories of leaders like Elon Musk, whose Tesla and SpaceX ventures are pushing the boundaries of possibility, and Jensen Huang, the visionary behind NVIDIA, who has revolutionized AI and computing.
Ian Khan at Davos: World Computer Day at Web3 Hub Davos 2025
Ian Khan will be participating in key events and moderating discussions that spotlight the intersection of technology, sustainability, and leadership. He will be moderating a session at the World Computer Day, at Web3 Hub Davos 2025, sharing his insights on how blockchain, Web3, and decentralized technologies are reshaping industries and empowering communities.
Meet Ian Khan at Davos
During the World Economic Forum 2025, Ian will hold a press tour in Davos to discuss Undisrupted, his vision for future readiness, and the role of innovation in addressing global challenges. This is a unique opportunity for journalists, industry leaders, and innovators to engage with one of the most influential voices in the field. Limited Advanced Reader copies of Undisrupted will be provided to confirmed media.
For one-on-one interviews, media inquiries and meeting requests, please contact:
Hannah Stephenapolis
PR Manager
[email protected]
When : Tuesday, January 20th- Jan 22nd 2025
Location : Davos, Switzerland
Tickets https://www.eventbrite.ca/e/futurist-ian-khans-undisrupted-book-launch-in-davos-tickets-1207873083909?aff=oddtdtcreator
Buy a Copy of Undisrupted at www.GetUndisrupted.com
#davos2025 #wef2025 #worldeconomicforum #wef2025 #davos #undisrupted #iankhanfuturist #thefuturist
Predictive Analytics in Business: What Futurists Say
By 2030, predictive analytics is projected to contribute over $40 billion in global revenue, reshaping industries like finance, retail, healthcare, and marketing with data-driven insights and decision-making (Statista). Predictive analytics, powered by AI, enables businesses to forecast trends, optimize operations, and drive strategic decisions. Keynote speakers provide insights into how predictive analytics is transforming business practices.
1. Andrew Ng: Co-founder of Coursera, Ng emphasizes predictive analytics in supply chain management. He explains how AI tools can forecast demand, optimize inventory, and enhance logistics, helping businesses reduce waste and increase efficiency. Ng advocates for integrating predictive models into every stage of the business cycle to make data-driven decisions that lead to better outcomes.
2. Fei-Fei Li: Co-director of the Stanford Human-Centered AI Institute, Li explores the role of predictive analytics in healthcare. She discusses how AI models can analyze medical data to predict patient outcomes, identify risk factors, and support preventive care, improving overall healthcare delivery. Li highlights the importance of ensuring that predictive models are ethical, fair, and transparent.
3. Sundar Pichai: CEO of Alphabet, Pichai highlights how Google uses predictive analytics to enhance user experience through personalized search results, recommendations, and ads. He explains how AI models anticipate user needs and adapt in real time, creating a seamless, more personalized interaction.
4. Eric Siegel: Author of Predictive Analytics: The Power to Predict Who Will Click, Buy, Lie, or Die, Siegel discusses the applications of predictive analytics in marketing. He highlights how AI systems analyze consumer behavior to predict purchasing patterns, helping businesses create targeted campaigns that maximize engagement and drive sales.
5. Kai-Fu Lee: Author of AI Superpowers, Lee explores predictive analytics in workforce management. He discusses how AI-driven tools can predict employee performance, enhance team dynamics, and optimize talent allocation, driving productivity and reducing turnover in businesses.
Applications and Challenges
Predictive analytics is driving transformation across industries, from customer behavior forecasting and demand prediction to risk management and resource allocation. However, challenges such as data privacy concerns, algorithmic bias, and the need for high-quality data remain. Keynote speakers stress the importance of robust data governance, transparency, and ethical AI practices in overcoming these hurdles.
Tangible Takeaway
Predictive analytics is revolutionizing decision-making in business by providing actionable insights based on data trends. Insights from leaders like Andrew Ng, Fei-Fei Li, and Sundar Pichai highlight its transformative potential. To maximize its benefits, businesses must prioritize data quality, ethical AI, and strategic integration across operations.
Keynote Speakers on Edge AI and Its Impact on IoT
By 2030, the global Edge AI market is projected to exceed $40 billion, driving innovations in the Internet of Things (IoT) by enabling real-time data processing at the edge of networks (Statista). Edge AI allows devices to make decisions locally, reducing latency, improving data privacy, and enhancing efficiency. Keynote speakers share insights into how Edge AI is transforming IoT and its future implications.
1. Sundar Pichai: CEO of Alphabet, Pichai highlights how Google’s Edge AI is enhancing IoT capabilities in smart homes and cities. He discusses how devices like Nest use real-time, on-device processing to optimize energy usage, increase security, and enhance user experiences without relying on centralized cloud systems.
2. Demis Hassabis: CEO of DeepMind, Hassabis explores how Edge AI is enhancing autonomous systems like drones and self-driving cars. He emphasizes how Edge AI enables these devices to process information in real-time, making decisions quickly and reliably, even in environments with limited connectivity.
3. Satya Nadella: CEO of Microsoft, Nadella focuses on how Azure IoT Edge empowers businesses to leverage AI at the edge, optimizing operations in industries like manufacturing and logistics. He explains how Edge AI allows companies to process data locally, predict equipment failures, and reduce downtime, driving efficiency and cost savings.
4. Fei-Fei Li: Co-director of the Stanford Human-Centered AI Institute, Li discusses how Edge AI is transforming healthcare. She explains how wearables and medical devices can monitor patients’ vital signs in real-time, providing immediate feedback and allowing for proactive care, improving patient outcomes and reducing hospital visits.
5. Dr. Fatih Birol: Executive Director of the International Energy Agency (IEA), Birol explores how Edge AI can optimize energy grids and consumption. He discusses how AI at the edge helps monitor and manage energy distribution efficiently, integrate renewable energy sources, and ensure reliable service.
Applications and Challenges
Edge AI is driving innovation in autonomous vehicles, healthcare, smart homes, and industrial automation. However, challenges such as high implementation costs, data security, and the need for efficient hardware remain. Keynote speakers advocate for advancements in processing power, secure deployment frameworks, and collaborative partnerships to unlock the full potential of Edge AI.
Tangible Takeaway
Edge AI is reshaping IoT by enabling real-time, secure, and efficient data processing. Insights from leaders like Sundar Pichai, Demis Hassabis, and Satya Nadella highlight its transformative potential across industries. To maximize its benefits, stakeholders must prioritize scalability, privacy, and innovative edge solutions.
Generative AI in Creativity: Keynote Speakers’ Perspectives
By 2030, the generative AI market is expected to surpass $200 billion, fundamentally reshaping the creative landscape across various sectors such as art, music, film, and design (Markets and Markets). Generative AI, which involves the creation of original content through algorithms trained on existing data, is transforming the way creativity is perceived and experienced. Visionary keynote speakers are leading discussions on how generative AI is not only enhancing creative processes but also empowering creators across industries.
Thought leaders like Sam Altman, CEO of OpenAI, and Kate Crawford, co-founder of the AI Now Institute, are at the forefront of AI in creativity. Sam Altman discusses how models like GPT and DALL-E are unlocking new creative possibilities, allowing artists, musicians, and writers to collaborate with AI in ways previously unimaginable. He highlights the ability of generative AI to create high-quality content quickly, enabling both established and emerging creators to produce innovative work on a large scale. Altman envisions a future where AI becomes a seamless part of the creative process, helping individuals realize their creative potential and expanding access to creativity for all.
Kate Crawford provides a critical perspective on the ethical implications of generative AI in the creative industries. She explores issues such as copyright, authenticity, and potential biases in AI-generated content. Crawford advocates for a more responsible and ethical development of AI tools that respect human creativity and ensure fairness in how AI systems generate and distribute creative works. She calls for transparency in AI’s use in creative fields, ensuring that AI-generated content does not perpetuate harmful stereotypes or exploit creators.
Applications of generative AI in creativity are vast and varied. In the visual arts, AI platforms like DALL-E and Artbreeder allow creators to generate entirely new pieces based on text prompts or images. In music, AI models are being used to compose songs, create unique soundscapes, and assist musicians in exploring new genres. In writing, tools like GPT-3 help authors with idea generation, content drafting, and editing, leading to new forms of storytelling. In fashion, generative AI can predict trends, design clothing, and optimize patterns, helping designers create innovative collections faster.
Keynotes also discuss the challenges of ensuring that AI-generated content adheres to intellectual property laws, the authenticity of AI-driven creations, and the potential to undermine human creativity. Speakers stress that generative AI should be seen as a tool to complement human creativity rather than replace it. Emerging trends include AI-assisted video creation, where AI helps create visual narratives, and the use of AI in game development, where it generates new characters, levels, and storylines, enhancing interactivity.
Takeaway? Generative AI is reshaping the creative landscape by empowering creators with new tools for self-expression and collaboration. Engaging with visionary keynote speakers equips technologists, artists, and business leaders with the insights to harness the full potential of generative AI while navigating ethical challenges, ensuring that these technologies enhance and enrich the creative process.
AI’s Impact on Energy Efficiency and Sustainability
By 2030, AI in energy is expected to contribute over $10 billion annually in energy savings, enhancing sustainability efforts through improved energy efficiency and better integration of renewable resources (Statista). AI is transforming the energy sector by optimizing energy consumption, predicting maintenance needs, and enabling real-time management of renewable energy sources. Keynote speakers discuss how AI is reshaping energy systems for a sustainable future.
1. Sundar Pichai: CEO of Alphabet, Pichai highlights Google’s use of AI to improve energy efficiency in its data centers, achieving a 30% reduction in energy usage. He discusses how AI can optimize energy consumption in other sectors, from smart homes to the grid, leading to a more sustainable world.
2. Demis Hassabis: CEO of DeepMind, Hassabis explains how AI is advancing energy efficiency by helping stabilize energy grids and balance supply and demand in real-time. He discusses DeepMind’s efforts to apply reinforcement learning to optimize energy consumption in cooling systems, reducing waste and improving sustainability.
3. Dr. Fatih Birol: Executive Director of the International Energy Agency (IEA), Birol discusses the role of AI in accelerating the transition to clean energy. He highlights how AI-powered forecasting tools are optimizing the deployment of renewable energy sources such as solar and wind, making the energy grid more reliable and efficient.
4. Fei-Fei Li: Co-director of the Stanford Human-Centered AI Institute, Li explores AI’s role in energy efficiency in smart buildings and cities. She emphasizes how AI systems can manage energy usage in real-time, adjusting lighting, heating, and cooling systems for maximum efficiency, reducing carbon footprints and operational costs.
5. Satya Nadella: CEO of Microsoft, Nadella highlights how Microsoft’s Azure AI platform is driving sustainability by enabling businesses to monitor energy usage and predict energy needs through predictive analytics. He discusses how AI is making energy-efficient technologies more accessible to organizations of all sizes.
Applications and Challenges
AI is enhancing energy efficiency and sustainability through smarter grids, predictive maintenance, and real-time energy optimization. However, challenges such as high implementation costs, data privacy concerns, and the integration of AI with existing energy systems remain. Keynote speakers advocate for collaborative industry efforts, regulatory support, and further research to unlock AI’s full potential in the energy sector.
Tangible Takeaway
AI is revolutionizing energy efficiency and sustainability by optimizing consumption, improving renewable energy integration, and reducing waste. Insights from leaders like Sundar Pichai, Demis Hassabis, and Dr. Fatih Birol underscore the importance of AI in achieving global sustainability goals. To fully realize AI’s impact, stakeholders must prioritize scalability, ethical development, and cross-sector collaboration.
